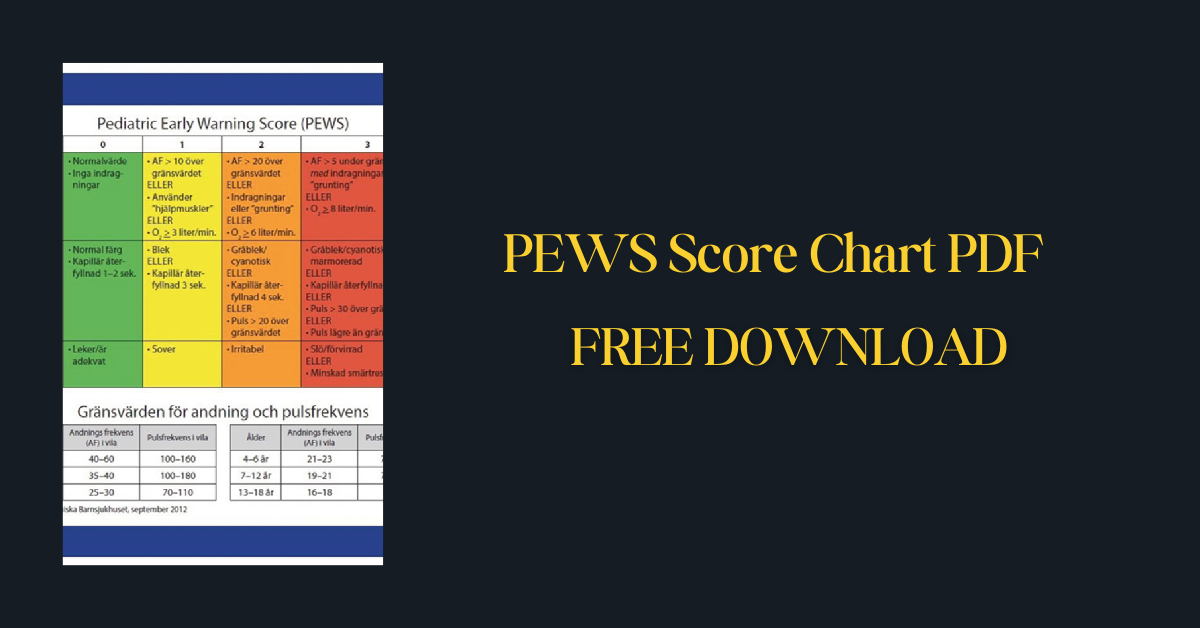
The Pediatric Early Warning Score (PEWS) is a vital tool utilized in pediatric healthcare settings to identify early signs of deterioration in a child’s condition. This scoring system provides healthcare professionals with a structured method for assessing a child’s clinical status, enabling timely intervention and potentially preventing adverse outcomes.
PEWS incorporates various physiological parameters such as heart rate, respiratory rate, blood pressure, and other clinical indicators to assign a numerical score. By regularly monitoring and interpreting these scores, healthcare providers can promptly escalate care as needed, ensuring the best possible outcomes for pediatric patients.
| Name of the PDF | PEWS Score Chart pdf |
| No. of pages | 2 |
| Category | |
| Language | English |
| PDF Link | Click Here |
Also Download
Chinese Diesel Heater Manual PDF
What is the PEWS Score Chart
PEWS stands for Pediatric Early Warning Score, and it’s a critical tool used by healthcare professionals to monitor and identify early signs of deterioration in children. A PEWS chart typically includes the following sections:
Age Bands: The charts are designed for specific age ranges, as physiological parameters differ based on child development. Common age bands include 0-11 months, 1-4 years, 5-11 years, and 12 years and above.
Physiological Parameters: The chart assesses several vital indicators:
- Behavior: Levels of alertness and interaction (e.g., playing, sleeping, irritable, lethargic).
- Cardiovascular: Skin color, capillary refill time, heart rate.
- Respiratory: Breathing rate, respiratory effort, oxygen requirements.
Scoring: Each parameter has a scoring system:
- 0: Within normal ranges
- 1-2: Mild to moderate deviation from the norm
- 3: Significant deviation, indicating high risk of deterioration.
The scores are added to give a total PEWS score. The higher the score, the greater the risk of a child’s condition deteriorating.
Importance of the PEWS Score Chart
Here’s why the PEWS (Pediatric Early Warning Score) Chart is so vital in pediatric healthcare:
Early Intervention for Better Outcomes
- Detecting Subtle Changes: PEWS charts track key physiological parameters with sensitivity. This means they can pick up on subtle changes in a child’s condition that could signal the beginning of deterioration.
- Prompting Timely Action: Because PEWS charts have clear escalation protocols tied to scores, healthcare providers know the precise actions to take at different risk levels. This prevents delays in treatment and supports timely interventions that can be lifesaving for children.
Standardization of Care
- Consistent Assessment: Across different care settings (wards, emergency rooms, etc.), PEWS provides a standardized approach to monitoring children. This means all healthcare professionals are essentially speaking the same language when assessing a child’s condition.
- Reducing Errors: By having a systematic tool, the PEWS chart helps reduce the risk of overlooking critical signs or misinterpreting individual observations.
Improved Communication and Teamwork
- Common Language: PEWS scores function as an instantly understood shorthand among healthcare providers. A nurse can quickly convey the level of concern by referring to the PEWS score, streamlining communication.
- Collaborative Decision-Making: As PEWS guides escalation, it facilitates coordination within the healthcare team. Doctors, nurses, and other specialists can work together more effectively to manage the child’s care.
Evidence-Based Practice
- Backed by Research: PEWS systems have been extensively studied and proven effective in various settings. Their use aligns with the best practices based on the latest medical research.
- Data for Quality Improvement: Hospitals can analyze PEWS data over time to identify trends and areas for further improvement in their pediatric care processes.
Why is PEWS Score Important
The PEWS (Pediatric Early Warning Score) Score is important for several crucial reasons:
- Sensitive Monitoring: PEWS tracks key physiological and behavioral indicators. This means subtle changes, which might be missed during routine observations, are flagged by the score.
- Preventing Adverse Events: Early detection of deteriorating health in children is critical. PEWS empowers healthcare professionals to intervene before a child’s condition becomes critical, reducing the risk of complications, serious illness, or even death.
- Consistent Care Across Settings: PEWS brings a structured approach to pediatric assessment across different care environments like hospitals, clinics, or emergency departments. This ensures every child receives consistent monitoring regardless of location.
- Clear Escalation Protocols: Tied to the PEWS score are specific escalation protocols. These guide healthcare professionals on precise actions to take –more frequent monitoring, calling a doctor, or immediate intervention – based on the level of risk. This streamlines response and reduces delays.
- Objective Measure of Risk: PEWS scores provide an objective way to understand a child’s condition. This makes communication between nurses, doctors, and other specialists more efficient and precise.
- Facilitates Teamwork: The clarity surrounding PEWS scores and escalation protocols enhances teamwork. Everyone involved in the child’s care is on the same page, fostering timely and well-coordinated interventions.
- Supported by Research: The use of PEWS systems is backed by extensive research. They have proven effective in reducing critical events and improving outcomes for children in various clinical settings.
- Informing Quality Improvement: The data generated through PEWS scores can be used to analyze trends within healthcare facilities and identify areas where processes can be further optimized for better pediatric care.
Components of PEWS Score
Here’s a breakdown of the typical components found in a PEWS Score chart:
Behavior: This section assesses the child’s level of alertness, interaction, and responsiveness.
Scoring:
- 0: Normal, age-appropriate behavior (awake, playful, interactive)
- 1: Sleeping, but easily woken
- 2: Irritable, restless, or difficult to console
- 3: Lethargic, reduced response to stimuli, or confused
Cardiovascular: Evaluates heart function and circulation through skin color, capillary refill time, and heart rate.
Scoring:
- 0: Pink skin color, capillary refill time under 2 seconds
- 1: Pale skin or prolonged capillary refill (around 3 seconds)
- 2: Mottled or gray skin, capillary refill 4-5 seconds, or mild tachycardia (heart rate slightly above normal)
- 3: Very mottled or gray skin, capillary refill over 5 seconds, significant tachycardia, or bradycardia (heart rate significantly below normal)
Respiratory: Assesses breathing rate, respiratory effort, and oxygen requirements.
Scoring:
- 0: Normal breathing rate, no increased effort
- 1: Elevated breathing rate, signs of mild respiratory effort (e.g., use of accessory muscles) or supplemental oxygen required
- 2: Significantly increased respiratory rate, signs of respiratory distress (e.g., retractions), or higher levels of oxygen support
Other Components (May Vary)
Some PEWS systems might include additional components like:
- Temperature: Whether the child has a fever or is hypothermic.
- Blood Pressure: Although not always included, significant changes can signal deterioration.
- Other Observations: Specific to the child’s condition, such as oxygen saturation levels, blood glucose levels, or neurological status.
How to Interpret a PEWS Score Chart
The PEWS score provides a standardized method for assessing a child’s overall clinical condition and determining the need for escalation of care or intervention. Here’s how to interpret the PEWS Score Chart:
Physiological parameters: The chart typically lists several physiological parameters along the rows, such as heart rate, respiratory rate, oxygen saturation, temperature, and level of consciousness.
Score assignment: For each parameter, there is a range of values corresponding to different numerical scores. Higher scores indicate a greater deviation from normal values, suggesting a potential clinical deterioration.
Age-specific ranges: The ranges for each parameter are often adjusted based on the child’s age, as normal physiological values can vary across different age groups.
Total score calculation: The scores for each parameter are added together to obtain a total PEWS score. Higher total scores indicate a higher risk of clinical deterioration.
Interpretation and action: The PEWS score is typically categorized into different risk levels or zones, such as low, medium, and high risk. Each zone corresponds to specific actions or interventions recommended by the healthcare institution or clinical guidelines.
For example:
- Low risk (PEWS score of 0-2): Typically indicates a stable condition, and routine monitoring may be appropriate.
- Medium risk (PEWS score of 3-4): May indicate early signs of clinical deterioration, and more frequent monitoring or additional assessments may be recommended.
- High risk (PEWS score of 5 or higher): Suggests a significant risk of clinical deterioration, and urgent medical evaluation or escalation of care may be required.
It’s important to note that the PEWS score should be interpreted in conjunction with the overall clinical assessment and judgment of the healthcare provider. The score is a tool to aid in decision-making but does not replace clinical expertise and consideration of the patient’s specific circumstances.
How is PEWS Score Implemented in Healthcare
The PEWS (Pediatric Early Warning Score) system is implemented in healthcare settings to facilitate early recognition of clinical deterioration in pediatric patients and prompt appropriate interventions. Here are some key aspects of how PEWS is implemented:
- Institutional protocols and guidelines: Healthcare institutions develop specific protocols and guidelines for the implementation and use of the PEWS system. These protocols outline the scoring criteria, the thresholds for different risk levels, and the corresponding actions or escalation pathways.
- Electronic medical records (EMR) integration: Many hospitals integrate the PEWS scoring system into their electronic medical records (EMR) or patient monitoring systems. This allows for automated calculation of the PEWS score based on the recorded vital signs and other clinical parameters.
- Nursing assessments and documentation: Nurses play a crucial role in implementing the PEWS system. During routine assessments, they measure and document the necessary physiological parameters, such as heart rate, respiratory rate, oxygen saturation, and level of consciousness. These values are then used to calculate the PEWS score.
- Monitoring and escalation: Based on the calculated PEWS score and the established thresholds, healthcare providers can determine the appropriate level of monitoring or escalation required for the patient. For example, a high PEWS score may trigger a rapid response team activation or transfer to a higher level of care.
- Multidisciplinary communication: Effective communication among the healthcare team, including nurses, physicians, and rapid response teams, is essential for the successful implementation of the PEWS system. Clear communication channels and protocols ensure that critical information is shared promptly and appropriate actions are taken.
- Education and training: Healthcare institutions provide education and training to staff members on the use of the PEWS system, interpretation of scores, and the appropriate responses for different risk levels. This training helps ensure consistent application and understanding of the system.
- Quality improvement and audits: Regular audits and quality improvement initiatives are undertaken to evaluate the effectiveness of the PEWS system, identify areas for improvement, and ensure compliance with established protocols.
- Customization and adaptation: While many institutions use standardized PEWS scoring systems, some may adapt or customize the scoring criteria or thresholds based on their specific patient population, local guidelines, or institutional preferences.
The successful implementation of the PEWS system requires a multidisciplinary approach, clear protocols, ongoing education, and a commitment to improving patient safety and outcomes through early recognition and appropriate management of clinical deterioration in pediatric patients.
Limitations of the PEWS Score
While the PEWS (Pediatric Early Warning Score) system is a valuable tool for identifying clinical deterioration in pediatric patients, it has several limitations that should be considered:
- Reliance on vital signs: The PEWS score primarily relies on physiological parameters, such as heart rate, respiratory rate, and oxygen saturation. However, it may not accurately reflect the overall clinical condition of a patient, especially in cases where the patient’s vital signs are not significantly abnormal but other clinical signs or symptoms are present.
- Subjectivity in scoring: Some parameters, such as level of consciousness or respiratory effort, may be subject to interpretation and can vary among healthcare providers. This subjectivity can lead to inconsistencies in scoring and potentially affect the accuracy of the PEWS score.
- Age-related limitations: The PEWS scoring system may not be equally accurate across all age groups, particularly for neonates or infants, as their physiological parameters and ranges can differ significantly from older children.
- Condition-specific limitations: The PEWS score may not be as sensitive or specific for certain medical conditions or patient populations. For example, patients with chronic respiratory conditions may have chronically abnormal vital signs, making it challenging to interpret the PEWS score accurately.
- Delay in recognition: While the PEWS system aims to facilitate early recognition of clinical deterioration, there can still be a delay between the onset of deterioration and the manifestation of abnormal vital signs or PEWS score changes.
- Reliance on accurate documentation: The accuracy of the PEWS score depends on the accurate and timely documentation of vital signs and clinical parameters by healthcare providers. Incomplete or inaccurate documentation can lead to incorrect PEWS scores.
- Lack of standardization: Different healthcare institutions may use slightly different PEWS scoring systems, scoring criteria, or thresholds, which can make it challenging to compare scores or interpret them consistently across different settings.
- Over Reliance on the score: While the PEWS score is a valuable tool, it should not be used as the sole determinant for clinical decision-making. Healthcare providers should consider the PEWS score in conjunction with a comprehensive clinical assessment, patient history, and their professional judgment.
To mitigate these limitations, healthcare institutions should provide ongoing training and education for staff, regularly review and update their PEWS protocols, and encourage a culture of critical thinking and clinical judgment in addition to using the PEWS score as a screening tool.
Additionally, research efforts continue to refine and improve the PEWS system to enhance its accuracy and applicability across different patient populations and clinical scenarios.
Conclusion
The Pediatric Early Warning Score (PEWS) chart serves as a vital tool in pediatric healthcare settings for early identification and intervention in deteriorating patients.
By utilizing a standardized scoring system based on clinical observations, vital signs, and other key parameters, healthcare providers can promptly recognize signs of clinical deterioration in children, allowing for timely interventions and improved patient outcomes.
The PEWS chart not only facilitates communication among healthcare team members but also empowers caregivers to escalate care appropriately when necessary.
FAQs
What is the purpose of the PEWS score chart?
The PEWS score chart is a tool used to help healthcare providers identify early signs of clinical deterioration in pediatric patients. It assigns numerical scores to various physiological parameters, allowing for a standardized assessment of the patient’s overall condition.
What parameters are included in the PEWS score chart?
Commonly included parameters are heart rate, respiratory rate, oxygen saturation, temperature, blood pressure, and level of consciousness. The specific parameters and their scoring ranges may vary across different healthcare institutions.
Are the score ranges the same for all age groups?
No, the score ranges for each parameter are often adjusted based on the child’s age, as normal physiological values can vary across different age groups (e.g., infants, toddlers, school-aged children, etc.).
How is the total PEWS score calculated?
The scores for each individual parameter are added together to obtain the total PEWS score. Higher scores indicate a greater deviation from normal values and a potentially higher risk of clinical deterioration.
What do the different PEWS score levels mean?
Typically, the PEWS scores are categorized into different risk levels or zones, such as low, medium, and high risk. Each level corresponds to specific actions or interventions recommended by the healthcare institution or clinical guidelines.
Is the PEWS score the only factor considered for clinical decision-making?
No, the PEWS score should be interpreted in conjunction with the overall clinical assessment and judgment of the healthcare provider. It is a tool to aid decision-making but does not replace clinical expertise and consideration of the patient’s specific circumstances.
Can the PEWS score chart be customized?
Yes, some healthcare institutions may adapt or customize the PEWS score chart to better suit their specific patient population, local guidelines, or institutional preferences.
How often should the PEWS score be documented?
The frequency of PEWS score documentation may vary based on the patient’s condition and institutional protocols. It is often documented during routine nursing assessments or when there is a change in the patient’s clinical status.
Is the PEWS score chart used only for inpatients?
While the PEWS score chart is commonly used in inpatient settings, it may also be employed in other healthcare environments, such as emergency departments or outpatient clinics, to aid in the assessment and triage of pediatric patients.
How is the PEWS score chart different from other early warning score systems?
The PEWS score chart is specifically designed for use in pediatric patients, while other early warning score systems, such as the Modified Early Warning Score (MEWS) or National Early Warning Score (NEWS), are intended for adult patients.

Niketa Mulay, a seasoned content writer and editor, has over a decade of experience. With a Master’s in Journalism, she honed her skills at The Times of India and now freelances across various industries. Passionate about reading, writing, and scuba diving, she shares expert PDF guides and tips at PDFdrivehub.com.